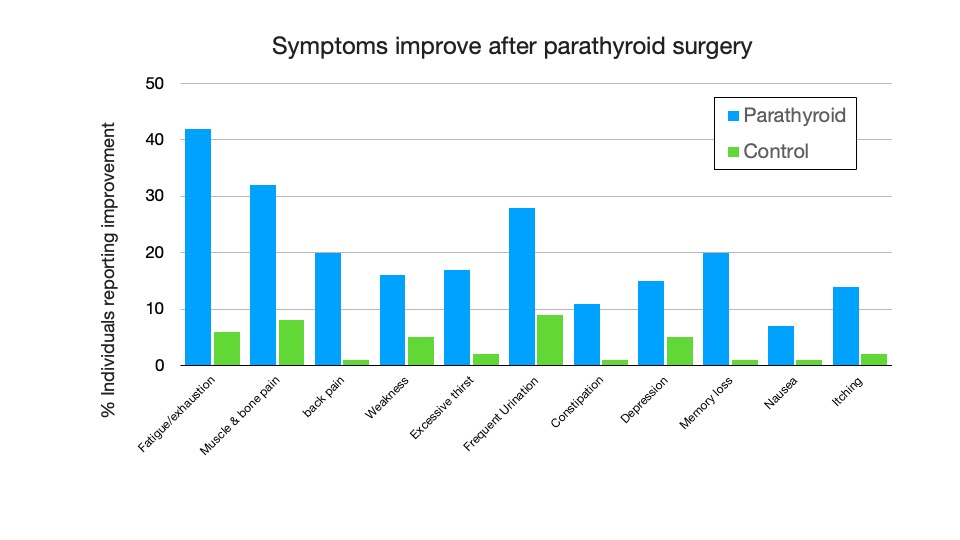
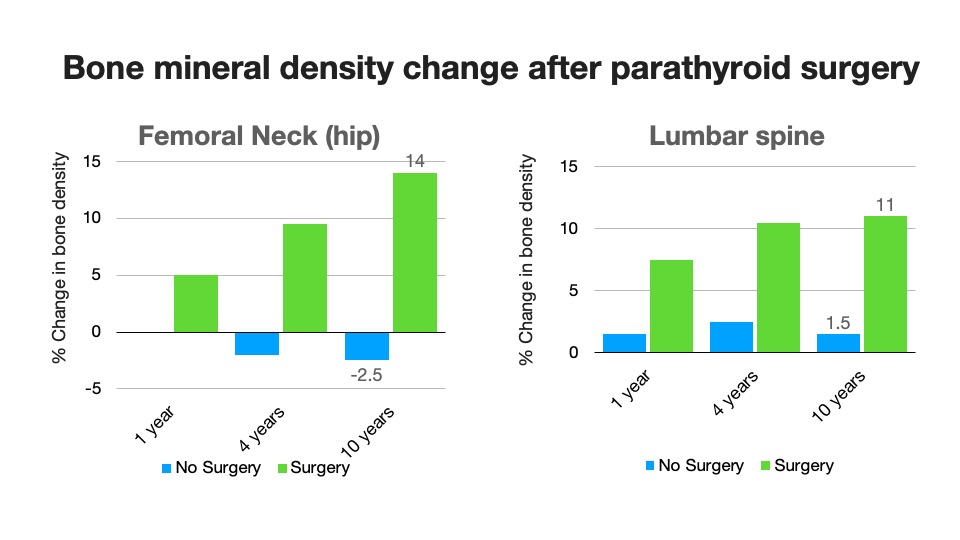
Does successful surgery improve these symptoms?
The graph here demonstrates what symptoms improved and by how much with successful parathyroid surgery. This paper was based on a large amount of data but it is still hard to know what symptoms are going to get better and how much by in any individual. These patients may have reported some improvement but how much?
2 good quality research papers from Oxford, UK and Calgary, Canada found a way of answering that. By formally quantifying quality of life scores it was shown that a patient’s perception of their quality of life improved significantly after surgery that cured them of HPT in over 70% of patients.